Abstract
Introduction: The role of T cell receptor (TCR) γδ cells in allogeneic hematopoietic stem cell transplantation (HSCT) is becoming of increasing interest1,2. In contrast to conventional alloreactive TCR αβ cells, TCR γδ cells are believed to have anti-tumor effects without causing graft-versus-host disease (GVHD). We conducted a single-center, prospective study to assess the impact of early TCR γδ cell immune reconstitution on overall survival, relapse and acute GVHD after HSCT.
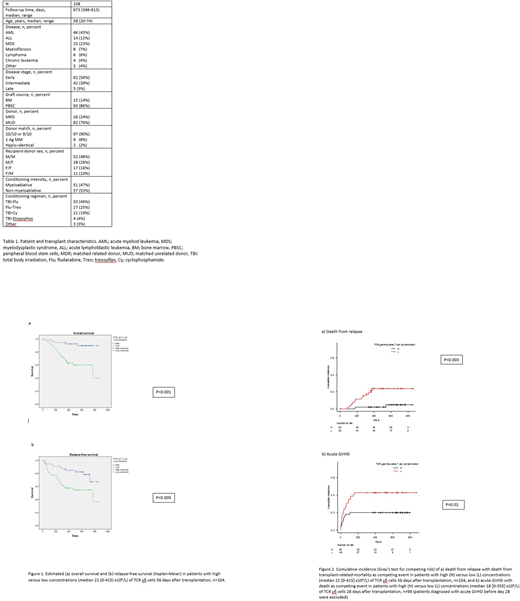
Methods: From October 2015 to March 2017, 108 consecutive patients transplanted for malignant diseases at the Bone Marrow Transplant Unit, Department of Hematology, Copenhagen University Hospital, Rigshospitalet, were included in the study, table 1. Fresh blood samples days 28, 56, 91, 180 and 360 after transplantation were analyzed for absolute concentrations of CD3-, CD4- and CD8 positive T cells together with a multi-color flow cytometry panel with staining for TCRαβ, TCRγδ, Vδ1, Vδ2, CD3, CD4, CD8, HLA-DR, CD196, CD45RO, CD45RA, CD16, CD56, CD314 (NKG2D) and CD337 (NKp30) for immune phenotyping.
Results: After a median of 673 (386-913) days, 28 (26%) patients had died from relapse (n=14) and from transplant-related-mortality(n=14), respectively. A total of 24 (22%) patients experienced relapse during the observation time with median time to relapse of 177 (56-778) days. Acute GVHD grade 2-4 was diagnosed in 38 (35%) of patients. Patients were divided into two groups by dichotomization at the median value of TCR γδ cell concentrations for Kaplan-Meier analyses of overall survival (OS), relapse-free survival (RFS) and cumulative incidence analyses (Gray's test for competing risks) of relapse and acute GVHD. Patients with high concentrations of TCR γδ cells 56 days after transplantation had significantly higher OS and RFS compared with patients with low concentrations, p<0.001 and p=0.005, respectively, figure 1. In Cox regression analyses with TCR γδ cell concentrations included as (log2-transformed) continuous variables, increasing concentrations of TCR γδ cells were significantly associated with increased OS and RFS, 0.72 (95% CI 0.58-0.87), p=0.001 and 0.82 (95% CI 0.68-0.98), p=0.03, respectively. High concentrations of TCR γδ cells remained significantly associated with increased OS and RFS in Cox regression multivariate analysis adjusted for disease stage at transplantation and conditioning regimen, 0.66 (95% CI 0.53-0.683), p<0.001 (OS) and 0.79 (CI 95% 0.65-0.95), p=0.01 (RFS), respectively. In cumulative incidence analyses of death from relapse with death from transplant-related-mortality as a competing event, patients with high concentrations of TCR γδ cells 56 days after transplantation had a significantly lower risk of dying from relapse compared to patients with low concentrations, p=0.003, figure 2a. Cumulative incidence of acute GVHD with death as a competing event furthermore showed that patients with high concentrations of TCR γδ cells 28 days after transplantation had significantly less acute GVHD compared with patients with low concentrations, p=0.02, figure 2b. All associations between TCR γδ cell concentrations and outcomes were independent of the total CD3 T cell concentrations.
Conclusion: The results of this prospective study suggest a protective effect of early robust TCR γδ cell immune reconstitution on relapse and acute GVHD resulting in increased OS after HSCT, and support further research in adoptive TCR γδ cell therapy in transplant patients.
Handgretinger, R. & Schilbach, K. The potential role of gd T cells after allogeneic HCT for leukemia. Blood131, 1063-1072 (2018).
Scheper, W., Grunder, C., Straetemans, T., Sebestyen, Z. & Kuball, J. Hunting for clinical translation with innate-like immune cells and their receptors. Leukemia28, 1181-1190 (2014).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal